Welcome
Welcome to McMaster’s Adult Nephrology Subspecialty Residency Program.
The McMaster University Nephrology Residency Program is a competency-based training program that has a strong emphasis on providing a comprehensive learning experience in order to achieve skills in all CanMEDS domains. The curriculum is unique and aimed to provide exposure to all aspects of nephrology, yet allowing for flexibility and self-directed learning. The program is tailored to learner needs and therefore a variety of assessment methods are utilized in order to provide trainees feedback and guidance. The academic half-day is novel and graded with PGY4 and PGY5 residents being provided separate and protected academic half-days. The faculty are extremely motivated and dedicated to resident learning and oversee all aspects of education.
The Nephrology Program at McMaster University and St. Joseph’s Healthcare Hamilton is the largest clinical program in Canada and therefore the residents are exposed to a highly complex pool of patients with a variety of renal diseases. In addition, there is a large renal transplant program that performs living, deceased donor and high-risk transplantation and has associated with it a large renal transplant outpatient clinic. The program emphasizes full patient care including an emphasis on nephrologists performing procedures.
The academic program also has a strong clinical, basic science and medical education research component. There are numerous renowned faculty within the Division of Nephrology who lead major research projects and are leaders in their field. A strong research infrastructure to support trainees in pursuing either clinical, basic science or medical education research is provided. In addition, residents are provided training in completing a quality improvement and patient safety project.
Entry Requirements
- For graduates from Canadian and US Internal Medicine training programs, please refer to the CaRMS Medicine Subspecialty Match (MSM website).
- For graduates from foreign Internal Medicine training programs, please provide the following:
- Curriculum Vitae (CV/Resume).
- Source of funding.
- Letter of interest indicating reasons for wishing to train at McMaster in Nephrology.
Application deadline
- For graduates from Canadian and US Internal Medicine training programs, please refer to our CaRMS website.
- For graduates from foreign Internal Medicine training programs, the deadline is December 1 prior to entry into the upcoming academic year which starts on July 1st.
Program Overview
The McMaster University Nephrology Training program’s core objective is to mentor graduate trainees who are practical and competent Nephrology consultants. There is a strong emphasis on contextually acquiring knowledge to help integrate and consolidate knowledge in developing competencies in renal-related problems and diagnostic procedures.
Being a resident-focused program, the goal is to accommodate the resident’s chosen career path and the program has been successful in tailoring a career targeted towards either academic or community-based nephrology.
Objectives
For the training program, core requirements will consist of the following. These occur in a four-week block rotation.
| PGY4 Year | PGY5 Year | |||
| 1 | Clinics I (General/Urgent Consult/Specialized Clinics) | 1 | AKI City Junior Attending |
|
| 2 | Dialysis Home Therapies I |
2 | Elective | |
| 3 | In patient Nephrology I |
3 | Transplant Clinics |
|
| 4 | Research | 4 | Competence Committee Selective |
|
| 5 | In patient Transplant Nephrology I |
5 | Inpatient Nephrology Junior Attending |
|
| 6 | Clinics II (General/Urgent Consult/Specialized Clinics) | 6 | Transplant Junior Attending |
|
| 7 | Clinics/Holiday Rotation | 7 | Clinics/Holiday rotation | |
| 8 | Competence Committee Selective | 8 | Pediatrics Obstetrical Nephrology |
|
| 9 | Acute Kidney Injury (AKI) -City |
9 | Research | |
| 10 | Nephropathology | 10 | Dialysis Home Therapies III |
|
| 11 | In patient Transplant Nephrology II |
11 | Clinics III (General/Urgent Consult/Specialized Clinics) | |
| 12 | Dialysis Home Therapies II |
12 | Elective | |
| 13 | In patient Nephrology II |
13 | Elective |
Phase Timelines
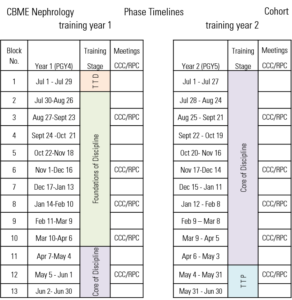
Expandable List
- Training Year One (PGY4)
- Training Stage TTD
- July 1 to July 29
- Training Stage Foundations of Discipline
- July 30 to August 26
- August 27 to September 23 (CCC/RPC Meeting)
- September 24 to October 21
- October 22 to November 18
- November 19 to December 16 (CCC/RPC Meeting)
- December 17 to January 13
- January 14 to February 10 (CCC/RPC Meeting)
- February 11 to March 9
- March 10 to April 6 (CCC/RPC Meeting)
- Training Stage Core of Discipline
- April 7 to May 4
- May 5 to June 1 (CCC/RPC Meeting)
- June 2 to June 30
- Training Stage TTD
- Training Year Two (PGY5)
- Training Stage Core of Discipline
- July 1 to July 27
- July 28 to August 24
- August 25 to September 21 (CCC/RPC Meeting)
- September 22 to October 19
- October 20 to November 16
- November 17 to December 14 (CCC/RPC Meeting)
- December 15 to January 11
- January 12 to February 8 (CCC/RPC Meeting)
- February 9 to March 8
- March 9 to April 5 (CCC/RPC Meeting)
- April 6 to May 3
- Training Stage TTP
- May 4 to May 31 (CCC/RPC Meeting)
- May 31 to June 30
- Training Stage Core of Discipline
Curriculum
Academic Curriculum
- Protected Academic Half Days for PGY4 (weekly): 2 sessions per academic half-day (3-4 hours in duration) are provided by faculty to trainees. The format is either lecture-based and/or case-based learning.
- Protected Academic Half Day PGY5 (weekly): 2 sessions per academic half-day and one session of case-based learning (4 hours in duration) are provided by faculty to trainees. The format is either lecture-based or case-based learning.
- Evidence-based Tuesday noon rounds (weekly)
- Nephrology Grand Rounds (weekly)
- Renal Clinical Pathology Rounds (monthly)
- Research Rounds (every 2 weeks)
- Nephrology Journal Club (every 2 months)
- Transplant Journal Club (every 6 months)
- Visiting professor rounds (4 times/year)
- Quality Improvement and Patient Safety Round (every 3 months)
- Combined Medicine Subspecialty Rounds (every 3 months)
- Simulation-based learning (every 6 months)
Procedure Based Curriculum
- Hemodialysis central venous catheter insertion
- Native and Renal Transplant biopsies
- Peritoneal dialysis catheter insertion (optional)
- Plasmapheresis
Clinical and Contextual Learning Curriculum
- Longitudinal clinics
- Hemodialysis clinics
- Peritoneal Dialysis clinics
- Vascular Access clinics
- Pretransplant clinics
- Post Renal Transplant clinics
- Living Donor clinics
- Specialty clinics (Glomerulonephritis, Vasculitis, Hypertension, Genetics, Obstetrical Nephrology, Transition, Transplant)
- Virtual Care Clinics
Research Curriculum
The Nephrology program has a strong research infrastructure to support trainees in pursuing either clinical, basic science or medical education research. Numerous faculty members of the division have an interest in various aspects of nephrology.
Additional information regarding the Division of Nephrology’s research productivity can be found on the Hamilton Centre for Kidney Research website.
