Welcome to the McMaster University Royal College Emergency Medicine Residency Program!
Hamilton is located in Southern Ontario and is in close proximity to other major cities including Toronto, Kitchener-Waterloo and the beautiful Niagara Region. Hamilton itself is home to a remarkable Arts and Culture Scene, Restaurants, and nature. Regardless of your interests, we can assure you that you can find it in Hamilton. Hamilton as a city is home to a huge spectrum of people of multiple ethnicities, socioeconomic statuses, and medical needs. We also serve as the regional center for an area of nearly 2 million people.
- Looking for the CCFP-EM Program – https://fammedmcmaster.ca/about-us/divisions/emergency-medicine/
- Looking for Clerkship electives – email ugemerg@mcmaster.ca
- Junior Resident (PGY1/2) Electives – email emctu@mcmaster.ca
- Senior Resident Electives (PGY3+) – email pardhaa@mcmaster.ca
We can’t wait to meet you!
- Dr. Alim Pardhan – Program Director – pardhaa@mcmaster.ca
- Dr. Kelly van Diepen – Assistant Program Director – kelly.vandiepen@medportal.ca
- Dr. Caillin Langmann – Assistant Program Director – langmac@mcmaster.ca
Program Contacts:
- Program Admin – Julia Smerilli – pgemerg@mcmaster.ca
- Program Manager – Teresa Vallera – vallera@mcmaster.ca
Why Choose McMaster University Emergency Medicine?
In the Hamilton region, over 200,000 people receive quality emergency medical care each year thanks to the diverse network of physicians that were homegrown here. Our collaborative community, comprehensive curriculum, and flexible learning options attract top talent and stimulate improved patient care.
We are one of the largest Royal College Emergency Medicine Programs in the country, however, are still small enough that you will very quickly get to know all of the faculty, residents and staff in all of our departments. Our Faculty are world-class and come from a number of different backgrounds and have a huge spectrum of interests ranging from Pre-Hospital care, Quality Improvement, Point of Care Ultrasound (POCUS), Critical Care and Pediatric Emergency Medicine to name a few. Our Resident group is equally diverse and has a strong belief in equity, social justice, and are intimately involved in any program changes or improvements. We are responsive to resident feedback and a number of the amazing changes in our program have been Resident-driven projects. We have excellent working relationships with both our CCFP-EM Colleagues as well as our Pediatric Emergency Medicine group and host a number of events with all three groups to ensure good working relationships as well as good educational experiences for our residents.
Within Hamilton itself we have 4 Major Teaching hospitals and our residents spend time at all of these sites. In addition, our residents have the option (and are encouraged to) also spend time at one of several available busy community hospitals in our region depending on where their interests lie. Our program is structured in accordance with the Royal College Training Requirements for Emergency Medicine and has been using competency-based training prior to the official launch of Competency By Design by the Royal College. This meant that our faculty and residents were well prepared for the move to Competency Based Training.
-
-
- We host a weekly, fully protected Academic Half Day for all our residents on Thursday mornings with both faculty (70%) and resident (30%) speakers,
- A monthly journal club
- Year Specific Academic Sessions tailored to stage of training
- Boot camps at all the major transitions in Residency to ensure that our residents are well prepared for their rotations
- Attendance at PEM Rounds when on PEM
-
We have a recently developed Wellness Committee/Curriculum that is a resident-driven program to ensure that our residents have the tools and skills needed to thrive during residency.
In order to prepare our trainees for their exams, we hold several practice written exams every year including both locally created as well as national exams. We also organize biannual practice oral exams for our PGY2 and 3 residents and monthly exams for our exam writing cohort. Overall, this means that most of our residents have a full day of academic content per week about half the time.
Our residents have multiple opportunities to pursue their own interests during residency training. This can start as early as the start of residency depending on what the area of interest is. Our residents have formal time in PGY5 to pursue an Area of Focused Competence (PDF) which can be any area of interest that is related to EM or Medicine in general. This sometimes is a more traditional pathway such as Pediatric EM, Critical Care or Point of Care Ultrasound, but has also been new areas such as Narrative Medicine. Some of our residents have developed their own pathways for this time and we are happy to consider almost anything of interest to the resident if it will help them further their careers.
We are very proud of our program, our residents and our graduates and are happy to discuss them further. Our people, our residents and our faculty are the strength of our program. If you would like to speak to the Program Director or Assistant Program Director, please feel free to contact us at our information below. Our Chief Residents are also happy to meet with people who are interested in the program and can be reached at emchief@mcmaster.ca If you are interested in attending our Academic Half Day, please reach out to the chief residents who can arrange for you to do so.
A Word From Our Team
Uncover more about your experience at McMaster through key members of our faculty.
Located in Southern Ontario, Hamilton is in close proximity to other major cities including Toronto, Kitchener-Waterloo and the beautiful Niagara Region. In addition to a remarkable arts and culture scene, restaurants, and nature, Hamilton is home to a huge spectrum of people of multiple ethnicities, socioeconomic statuses, and medical needs.
About Us
At the Division of Emergency Medicine (EM), it’s our mission to foster world-class research, education, and leadership with a strong focus on clinical applicability. It’s our vision to be recognized as a centre of excellence for evidence-based practice and as a leader in clinical innovation, education, and research.
Our program objectives include:
- Improving patient care through excellence in EM education and research
- Building and strengthening a unified McMaster EM presence at local, national, and international levels
- Engaging in meaningful EM research and innovation
- Training and fostering EM leaders in clinical, educational, and research-oriented areas
Apply Now
While COVID-19 continues to challenge the way postgraduates and residents find their way to McMaster’s program, we’re still eager to connect and accept applications through a fair, objective, and transparent process.
Curriculum Structure
Clinical Curriculum
To ensure each student is fully equipped with the knowledge and skills required to successfully complete the EM program, our team has developed and continues to update an all-inclusive curriculum.
Curriculum Map 2020
Before beginning McMaster’s EM program, catch a glimpse of your educational journey. Our map provides incoming students with a detailed overview of the program’s yearly curriculum.
Entrustable Professional Activities (EPA) by Rotation
We believe experience is fundamental for building a diverse skill set. With EM’s five-year program, students experience hands-on, real-world learning through a rotational structure.
Electives
We are happy to meet with students who wish to speak to us about the program. If you are interested, please feel free to contact the PD or APD and we would be happy to set up a meeting:
Dr. Alim Pardhan – Program Director – pardhaa@mcmaster.ca
Dr. Kelly van Diepen – Assistant Program Director – kelly.vandiepen@medportal.ca
Dr. Caillin Langmann – Assistant Program Director – caillin.langmann@medportal.ca
Our Chief Residents are also happy to meet with people who are interested in the program and can be reached at emchief@mcmaster.ca If you are interested in virtually attending our Academic Half Day, please reach out to the chief residents who can arrange for you to do so.
Junior Resident Electives (PGY1/2) – Please contact emctu@mcmaster.ca
Senior Resident Electives (PGY3+) – Please contact Dr. Alim Pardhan at pardhaa@mcmaster.ca
AHD Schedule
Competency-Based Learning
Transition to CBME
Residents who began their Emergency Medicine training in 2018 at McMaster were the first large cohort of residents training in the CBD model. With pre-planning and our amazing resident group, it has been a smooth and successful transition.
CBD will use exposures rather than time as the basis for progression. It is not anticipated that the duration of training will change for the majority of trainees. Residency programs will be broken down into stages, and each stage will have a series of milestones based on required competencies. These milestones will create more targeted learning outcomes and involve more frequent, formative assessments within the clinical workplace to ensure residents are developing and receiving feedback on the skills they need.
The Specialty Committee at the Royal College has developed:
-
-
- Entrustable Professional Activities (EPAs). EPAs are cardinal tasks that are required to become a competent emergency physician. EPAs will form the basis of evaluation and promotion in the Competency-Based Education Model.
- Required training experiences will help determine which rotations/experiences residents must undertake.
-
The new stages for residency programs under CBD are:
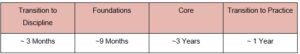
Note: Transition between stages will take place once the requisite competencies in a particular stage have been completed.
We have also implemented a highly-rated, new Academic Half Day curriculum, bootcamp series, administration and CQI curriculum in conjunction with CBD.
CBME has resulted in:
-
-
- Fewer off-service rotations
- Modifications to off-service rotations to maximize their relevancy to EM
- A program that will be more tailored to individual residents
-
The Exam will take place after the core stage. Transition to Practice will also include time for training in an Area of Focused Competence.
Remember: What you need to learn to be a safe and competent Emergency Physician has not changed at all. We may be putting some new labels on things and grouping them in different ways, but the job itself has not changed as a result of CBD. Rest assured that the program will continue to train excellent emergency physicians under CBD.
Research
Approach
Research & Scholarship
The Objectives for Research for FRCPC EM Residents are:
-
-
- Be good consumers of research – both in terms of being able to find literature and resources relevant to their clinical practice as well as the ability to critically appraise this literature.
- Be able to complete a quality assurance or research project in whatever setting they happen to be working in.
- Be able to produce a scholarly project worthy of publication and presentation. This is achieved with the following:
-
PGY1 RESIDENTS
Completion of the emergency medicine research curriculum which teaches research design, planning, ethics, management, analysis and critical appraisal. By the end of this course, the residents will be competent at appraising research articles and will have produced their own unique systematic review (Bestbet).
PGY2 RESIDENTS
In PGY2 Residents complete their EMS Curriculum and CQI Curriculum. They are expected to complete a scholarly project in one of the following areas:
-
-
- CQI – EMS
- CQI – Other
- Other Research Project
-
Other Scholarly Work that is approved by the program
Horizontal Critical Appraisal & Evidence Update Journal Clubs
All residents are expected to attend Journal Club:
-
-
- 4 Critical Appraisal Sessions per year
- 4 Evidence Update Sessions per year Residents are expected to attend Journal Club Sessions when not on approved leave or post-call.
-
Other Research Involvement
Residents may choose to be involved in other research endeavours once they have completed their basic research training in PGY1. It is strongly recommended that any research projects be vetted by the Program Research Director to ensure that there is adequate supervision.
Past Projects
Safety
McMaster Emergency Medicine Safety Policy
Preamble
The Royal College of Physicians and Surgeons accreditation standards (B1.3.9) requires that every residency program have specific policies with respect to resident safety. The policy should allow residents discretion and judgment regarding their personal safety and ensure residents are appropriately supervised during all clinical encounters.
The document, Postgraduate Medical Education Health and Safety Policy available at: https://pgme.mcmaster.ca/app/uploads/2019/02/Health-Personal-Safety-Policy-PGEC-2011.pdf provides procedures for reporting and responding to specific circumstances contained in that document. The Emergency Medicine residency program formally acknowledges, endorses, and agrees to adhere to these guidelines.
Residents have the right to a safe environment during their residency training. The responsibility for promoting a culture and safe environment is shared between the University, the faculty of medicine, the hospitals/clinical departments, residency training programs and the residents themselves.
Key Responsibilities
FOR RESIDENTS
- To provide information and communicate safety concerns to the program and to comply with safety policies.
FOR RESIDENCY TRAINING PROGRAMS
- To act promptly to address identified safety concerns and incidents and to be proactive in providing a safe learning environment.
Physical Safety
These guidelines apply only during residents’ activities that are related to the execution of residency duties:
Travel Safety
- When residents are travelling for clinical or other academic assignments by private vehicle, it is expected that they maintain their vehicle adequately and travel with appropriate supplies and contact information. Provincial laws prohibit non-hands-free cell For phone use and text messaging in the performance of residency duties while driving.
- For long-distance travel for clinical or other academic assignments, residents should ensure that a colleague or the home residency office is aware of their itinerary.
- Residents should not be on call the day before long-distance travel for clinical or other academic assignments by car. When long-distance travel is required in order to begin a new rotation, the resident should request that they not be on call on the last day of the preceding rotation. If this cannot be arranged then there should be a designated travel day on the first day of the new rotation before the start of any clinical activities.
- Residents are not to be expected to travel long distances during inclement weather for clinical or other academic assignments. If such weather prevents travel, the resident is expected to contact the program office promptly. Assignment of an alternate activity is at the discretion of the Program Director.
Hospital Safety
- Residents are not expected to walk alone for any major or unsafe distances at night. This includes walking on the hospital premises and parking lots. The residents are expected to request security escorts if such circumstances occur. Residents should not drive home after call if they have not had adequate rest.
- Residents should not assess violent or psychotic patients without the backup of security and an awareness of accessible exits. When interacting with patients with a potential for violence, residents should ascertain that there is a backup from security staff and that the patients are seen in an area, which allows for safe and easy exit
- The physical space requirements for the management of violent patients must be provided where appropriate.
- Site orientations should include a review of local safety procedures.
Personal Safety
- Residents should only telephone patients using caller blocking.
- Residents should familiarize themselves with the location and services offered by the Employee Health and Safety/Occupational Health Office.
- HGH 4 North Room 415, ext. 46307
- JHCC Section A – Level 0 – Room 60, ext. 42314
- MUMC 1F11 (behind red elevators), ext. 75573
- SJHH Charlton (Martha Wing 4th Floor), ext. 33344
- This includes familiarity with policies and procedures for infection control and protocols following exposure to contaminated fluids, needle stick injuries, and reportable infectious diseases.
- Residents must observe universal precautions and isolation procedures when indicated.
- Residents should keep their immunizations up to date. Overseas travel immunizations and advice should be sought well in advance when travelling abroad for electives or meetings.
- Pregnant residents should be aware of specific risks to themselves and their fetus in the training environment and request accommodations where indicated. Residents should consult the Occupational Health Office for information.
Psychological Safety
- Learning environments must be free from intimidation, harassment, and discrimination. Where there are situations where there are concerns regarding Intimidation, harassment or discrimination residents are strongly encouraged to discuss this with the Program Director, Associate Program Director or Program Assistant. Residents may also contact the Post Grad Office directly.
- When a resident’s performance is affected or threatened by poor health or psychological conditions, (physical or mental) the resident should be granted a leave of absence and receive appropriate support. Such residents should not return to work until an appropriate assessor has declared them ready.
- Residents should be aware of and have easy access to the available sources of immediate and long-term help for psychological problems, substance abuse problems, harassment, and inequity issues.
Professional Safety
- Residents may experience conflicts between their ethical or religious beliefs and the training requirements and professional obligations of physicians. Resources should be made available to residents to deal with such conflicts. Examples include the Program Director, the Canadian Medical Protective Association and the College of Physicians and Surgeons of Ontario.
- Residents must be appropriately supervised recognizing that part of residency training is graded responsibility. Details regarding specific standards of supervision may be found on the CPSO Policy Professional Responsibilities in Postgraduate Medical Education – https://www.cpso.on.ca/Physicians/Policies-Guidance/Policies/Professional-Responsibilities-in-Postgraduate-Medi
- Where there is a disagreement between a resident and a faculty member with respect to the management of a patient, there is a process endorsed by McMaster University and the Council of Ontario Faculties of Medicine – https://cou.ca/wp-content/uploads/2017/10/Resolution-of-Resident-Conflict-with-Attending-Physician-or-Supervisor-on-an-Issue-of-Patient-Care.pdf
- The Program will adhere to the PARO-CAHO Collective Agreement.
- Where possible the Program will accommodate religious holidays having regard for professional and patient care responsibilities.
- Residents should have adequate support from the program following an adverse event or critical incident.
- Programs should promote a culture of safety in which residents are able to report and discuss adverse events, critical incidents, ‘near misses’, and patient safety concerns without fear of punishment.
- Residency program committee members must not divulge information regarding residents. It is the responsibility of the residency Program Directors to make the decision and to disclose information regarding residents (e.g. personal information and evaluations) outside of the residency program committee and to do so only when there is reasonable cause. The resident file is confidential.
- Resident feedback and complaints must be handled in a manner that ensures resident anonymity unless the resident explicitly consents otherwise.
- Residents must be members of the CMPA and follow CMPA recommendations in the case of real, threatened, or anticipated legal action.
The Role Of Residents in Ambulance Transports
PGE:COFM Dec. 9, 1999, Educational Principles
- In many programs, participation in patient transport is a valuable learning experience for residents.
- There must be clear educational objectives underlying the resident’s participation in patient transport.
- Residents must have appropriate training with demonstrated competency in the circumstances relevant to the transport experience.
- Communication and supervision between the resident and his/her designated supervising physician must be available at all times.
- Resident well-being should be considered in all transports.
Note: On occasion residents/fellows may be confronted with a situation for which they are not sufficiently trained. It is expected that they, like other physicians, will deal with such situations as practicing professionals to the best of their ability. The Program Director is always available to provide support and guidance.
Shift Reduction
PGY5 EM Shift Reductions Prior to Exams
In order to provide them with additional time to study for their Royal College Exams, FRCPCP EM Residents in PGY5 are provided with a shift reduction for the 3 blocks leading up to the exam until the exam is complete. As this shift reduction is intended to provide residents with additional time to study, it is understood that if a resident chooses to use the shift reduction, they will not pick up any additional clinical work during this period.
Shift Requirements
For the 3 Blocks leading up to the written exam, the shift requirement for PGY5 Residents is 11 shifts per block.
Starting in the block following the oral exam the shift requirement returns to 15 shifts per block.
Vacation Adjustments during the period of the shift reduction:
- 3 shift reduction for every 1 week of vacation
- Less than 1 week of vacation – 1 shift reduction for every 2 vacation/PL days
- Absolute minimum of 8 shifts in a block
Exam Blocks
The Block of the Written Exam:
- 2 Exam Days
- If Resident takes a week off – 8 Shifts Minimum
- If not – 10 shifts
The Block of the Oral Exam:
- 1 Exam Day + Travel time to and from Ottawa
- If Resident takes a week off – 9 shifts Minimum
- If Not – 11 Shifts
If both the Written and Oral Exams are in the Same Block:
- 3 Exam Days + Travel time to and from Ottawa for the Oral Exam
- If a Resident Takes a Week off – 6 Shifts Minimum
- If a Resident Takes 2 weeks off – 4 shift minimum
- If not – 8 shifts
If there is a full block between the Written and Oral Exam:
- 13 Shifts in that block
- 3 shift reduction for every 1 week of vacation
- Less than 1 week of vacation – 1 shift reduction for every 2 vacation/PL days
- Absolute minimum of 8 shifts in a block
Night shifts will not be required during the shift reduction period, however, residents may choose to work them if they so desire.
Residents need not have a preceptor for any block where they have 8 or fewer shits, however, will require one in any block with more than 8 shifts.
Any resident doing longitudinal PEM Shifts may only do 1 PEM Shift per block during the shift reduction period.
PGY5s are entitled to an additional week (7 days) of Professional Leave in the 4 weeks leading up to the Royal College exam. Residents may choose to split the 7 days between the written and oral components of the certification exam or take all 7 days consecutively.
Academic Requirements
Given the multiple roles of PGY5 residents at rounds, journal club and other academic events, it is expected that they will attend all academic events until 4 weeks in advance of the written exam and 1 week prior to the oral exam. This requirement does not apply if on a formal vacation or PL.
In the 4 weeks prior to the written exam (and 1 week prior to oral exam) PGY5 Residents are encouraged to come to academic events however it will not be required. Following the exams the attendance requirements return to normal.
Any unique circumstances not outlined above will be considered on a case-by-case basis by the program director.
Restricted Registration
The McMaster Emergency Medicine program is a participant in the provincial Restricted Registration (RR) program. The following is a summary of the yearly requirements that should be met by residents seeking RR licensing.
Please note that though you are eligible, you must independently apply for a special RR license through the CPSO registration committee. Please see the RR website for more information (http://restrictedregistrationontario.ca/).
Fees & deadlines: It is important to note that there are required fees and strict deadlines. Fees for an RR license must be paid on a yearly basis for each job site regardless of how much of the year is spent working.
Current eligible sites for eligible McMaster FRCPC ER Residents
- HGH ICU
- JH ICU
- SJH ICU
- MCH PCCU
Requirements for participation
- Attendance at AHD/JC meets expectations for good standing
- Adequate performance for CITE and Block Exams
- On Track for EPAs and other evaluations
Guidelines
- Can apply during PGY3 following Critical Care Rotations
- Limited to 1 additional shift per week
- Work hours can NOT exceed the maximum/time off between shifts as outlined in the PARO-CAHO Collective Agreement
- May not interfere with Residency Program Requirements (clinical or academic)
- May not be done during shift reduction period leading up to Royal College exam.
Equity, Diversity and Inclusion
McMaster University Emergency Medicine EDI Statement
McMaster University is located on the traditional territories of the Haudenosaunee and Mississauga Nations and, within the lands protected by the “Dish with One Spoon” wampum agreement.
In keeping with its Statement on Building an Inclusive Community with a Shared Purpose, McMaster University strives to embody the values of respect, collaboration and diversity, and has a strong commitment to employment equity. The diversity of our workforce is at the core of our innovation and creativity and strengthens our research and teaching excellence. The University seeks qualified candidates who share our commitment to equity, diversity and inclusion. All qualified candidates are invited to apply and we particularly welcome applications from women, persons with disabilities, First Nations, Métis and Inuit peoples, members of visible minorities, and LGBTQ+ persons.
The McMaster FRCPC Emergency Medicine Program in particular aims to build a community that is safe, inclusive, and respectful for all. We unequivocally condemn racism in all forms, and recognize that Black, Indigenous, and people of colour suffer disproportionate acts of hatred and discrimination. We stand in solidarity with our patients and colleagues who experience injustice and commit to creating a more tolerant reality.
As current and future Emergency Medicine practitioners we recognize the power and privilege we hold when caring for patients, often at their most vulnerable. We see the result of social inequality on a daily basis manifested as poor health outcomes. Advocacy should be a foundational component of our academic, research, and clinical work.
Our program pledges to embed this in the work that we do. We commit to continually reflecting, listening, learning, and, where needed, changing our systems. The Inclusion, Diversity, Equity, and Anti-racism (IDEA) committee is a group of McMaster EM residents with a dual focus on academic programming and on increasing representation in emergency medicine.
Our Teaching Hospitals

Hamilton General Hospital
- A high volume and very high acuity centre
- Has one of the province’s few inpatient burn units
- Recognized as a regional centre in cardiovascular care, neurosciences, trauma and burn treatment
- Level 1 Trauma Centre
- Stroke centre
McMaster Children’s Hospital and McMaster University Medical Centre
- Has one of the largest neonatal intensive care units in the province
- Regional pediatric trauma centre
- PED receives more than 50,000 visits a year
- Provides regional care for high-risk pregnancies
Juravinski Hospital
- Extensive redevelopment in 2012 including the Emergency Department
- Specializes in Cancer Care and Orthopedics, specifically joint replacement
- Cancer patients come from throughout the region to access specialized services
- New initiatives with focus on Geriatric EM
St. Joseph’s Hospital
- Regional leader in respiratory care, thoracic surgery, emergency psychiatry, and nephrology
- Regional leader for mental health and addiction services in south-central Ontario
- Has an extensive focus on research
Community ED Sites that our Residents work at regularly (electives are possible at other sites as well)
- Brampton Civic
- Grand River (KW)
- Trillium (Mississauga)
- Barrie
- Joe Brant (Burlington)
- St. Catherines General
Life in Hamilton
A Good Secret Is Hard To Keep…
The City of Hamilton is abundant with arts and culture, culinary delights, outdoor space, and entertainment options. Explore one of the links below to learn more about local favourites or visit Tourism Hamilton for a full overview of the City’s happenings.
Sports & Entertainment
- Hamilton Bulldogs
- Hamilton Tiger Cats
- First Ontario Centre
- The Studio
- The Westdale Theatre
- Starlite Drive-In
- Mills Hardware
Arts & Culture
Food & Drink
- The Snooty Fox
- Odds Bar
- 541 Eatery & Exchange
- Mezcal Tacos & Tequila
- Earth to Table Bread Bar
- The Burnt Tongue
- Uncle Ray’s Food & Liquor
- Saint James Espresso Bar & Eatery
- The Mulberry Coffeehouse
- HAMBRGR
- The Mule
- Berkeley North
- The French
- Saltlick Smokehouse
- Nique
- Bar Sazerac
- The Brain
- Merit Brewing
- Donut Monster
- Cake and Loaf
- SYNONYM
Outdoor Recreation
- Pier 4
- Gage Park
- Confederation Park
- Coote’s Paradise
- The Bruce Trail
- Chedoke Golf Course
- King’s Forest Golf Course
Events
(Collective Arts Annual Event)
Useful Resources
